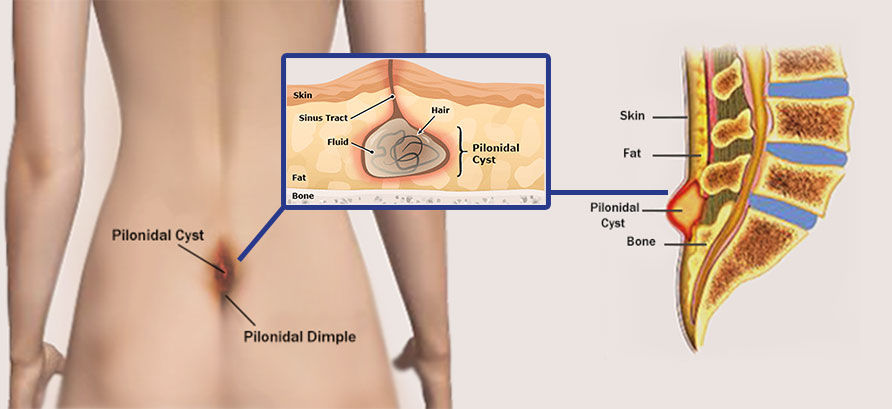
At North Shore Center For Plastic Surgery we can diagnose and offer treatment options for your pilonidal cyst. Typically treatment options include antibiotic management, emergency drainage of cyst or complete surgical removal.
Emergent Surgical Drainage
Surgical Removal and Reconstruction
Patients who experience repeated pilonidal abscesses, develop a chronic draining sinus, or have a recurrent cyst despite previous treatment will often require a complete surgical excision of the cyst and any associated infected tissue (a procedure called a pilonidal cystectomy).
Traditionally, the excised area was left open to heal on its own over time, a process that can take many months with wound care. Due to tension and moisture to the area, healing may be unpredictable and result in suboptimal outcomes. More advanced treatment involves creation of a tissue flap that has significantly improved healing and recovery.
Modified Limberg Flap
In this approach, a diamond-shaped incision is made around the cyst, incorporating any sinus tracts and diseased tissue connected with the cyst. An adjacent tissue flap is then harvested, rotated, and used to cover the defect without creating tension. The donor site of the flap is closed primarily. Flap coverage of the defect eliminates any open wounds and improves healing by keeping the incision away from the midline. Wound healing complications often seen with wounds left open in this area are greatly reduced.
This surgery is performed as an ambulatory surgery under anesthesia. Duration of surgery is approximately 1.5 hours. A surgical drain is placed under the flap area and removed in the office in one week. Pressure and stress to the flap area needs to be avoided for 3 weeks. Full healing is seen in 6-8 weeks.

